
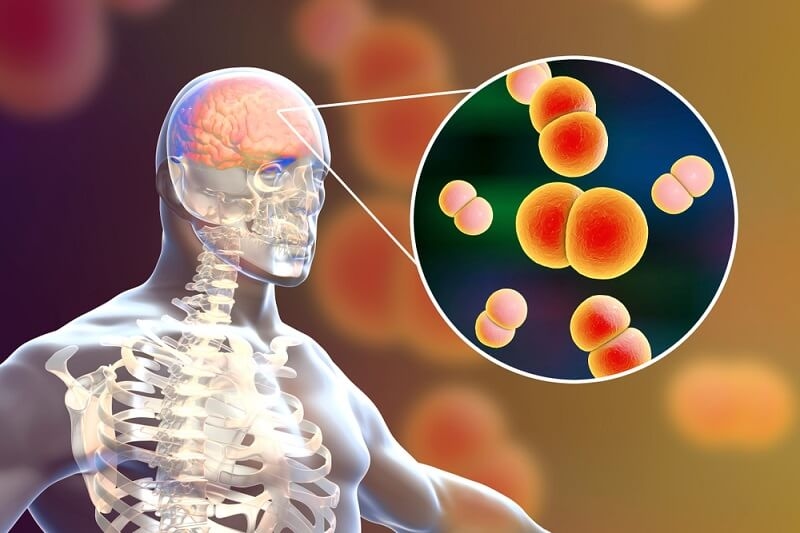
Meningitis is a serious medical condition characterized by inflammation of the protective membranes surrounding the brain and spinal cord. It can be caused by viral or bacterial infections, with bacterial meningitis being the more severe and potentially life-threatening form. The disease can affect individuals of all ages, but it is most commonly found in infants, children, and young adults. Meningitis is a medical emergency that requires prompt diagnosis and treatment to prevent serious complications.
Causes of Meningitis
Bacterial Meningitis
Bacterial infections are a leading cause of meningitis and are associated with severe and potentially life-threatening cases. Several bacteria can trigger bacterial meningitis, including:
a. Neisseria meningitidis: This bacterium is a common cause of meningococcal meningitis. It is transmitted through respiratory droplets and can lead to outbreaks, particularly in crowded settings such as college campuses or military barracks.
b. Streptococcus pneumoniae: Known as pneumococcus, this bacterium is a significant cause of bacterial meningitis, particularly in infants, older adults, and individuals with weakened immune systems.
c. Haemophilus influenzae: Before the introduction of the Hib vaccine, Haemophilus influenzae type b was a leading cause of meningitis in children. However, routine vaccination has significantly reduced its incidence.
Viral Meningitis
Viral infections are the most common cause of meningitis and are generally less severe than bacterial meningitis. Common viral pathogens responsible for viral meningitis include:
a. Enteroviruses: These viruses, such as coxsackieviruses and echoviruses, are responsible for the majority of viral meningitis cases. Enteroviruses are usually transmitted through contact with infected feces or respiratory secretions.
b. Herpesviruses: Certain herpesviruses, including herpes simplex virus type 1 (HSV-1) and varicella-zoster virus (VZV), can cause meningitis. These infections are often associated with other symptoms, such as oral or genital ulcers in the case of HSV-1 and chickenpox or shingles in the case of VZV.
Other Infectious Causes
Besides bacteria and viruses, other infectious agents can cause meningitis, although they are less common:
a. Fungal Infections: Fungal meningitis is typically associated with specific risk factors, such as a weakened immune system or exposure to certain environmental sources like contaminated soil or bird droppings. Cryptococcus neoformans is the most common fungal pathogen causing meningitis.
b. Parasitic Infections: Parasitic meningitis is rare but can occur in certain geographical regions. The parasite Naegleria fowleri, found in warm freshwater and soil, can cause a rare but often fatal form of meningitis.
Non-Infectious Causes
Meningitis can also be caused by non-infectious factors, including:
a. Drug Reactions: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and immunomodulatory drugs, have been associated with aseptic meningitis, which is characterized by similar symptoms to infectious meningitis but without the presence of bacteria or viruses.
b. Cancer: In rare cases, meningitis can be a complication of certain types of cancer, such as leukemia, lymphoma, or metastatic tumors that spread to the meninges.
c. Autoimmune Disorders: Some autoimmune disorders, such as lupus or Behcet's disease, can lead to meningitis due to an abnormal immune response targeting the protective membranes surrounding the brain and spinal cord.
Warning Signs of Meningitis You Should Never Ignore

High Fever: One of the hallmark symptoms of meningitis is a high fever. A sudden and persistent fever, often accompanied by chills and sweating, should raise concern, especially if there are other associated symptoms. A temperature above 101F (38.3C) may indicate an infection that requires immediate medical attention.
Severe Headache: A severe headache is a common symptom of meningitis. The headache may be intense, persistent, and often described as the worst headache ever experienced. It can be accompanied by sensitivity to light (photophobia) and sound, making it difficult to tolerate bright lights or loud noises.
Stiff Neck: Stiff neck or neck pain is another significant warning sign of meningitis. The inflammation of the meninges can cause neck muscles to become stiff and painful, limiting the range of motion. If attempting to touch the chin to the chest is met with resistance or severe discomfort, medical attention is necessary.
Altered Mental Status: Meningitis can affect cognitive function and mental status. Individuals may experience confusion, irritability, or difficulty concentrating. In more severe cases, there may be changes in consciousness, such as lethargy or even coma. Any sudden changes in mental status should be taken seriously and evaluated promptly.
Nausea and Vomiting: Nausea and vomiting are common symptoms of meningitis. The inflammation of the meninges can irritate the stomach and lead to gastrointestinal disturbances. If nausea and vomiting occur, particularly when accompanied by other warning signs, medical evaluation is essential.
Skin Rash: In certain types of meningitis, such as meningococcal meningitis, a characteristic skin rash may develop. This rash typically appears as small, reddish-purple spots or bruises and may not fade when pressed with a glass (a sign of meningococcal sepsis). The presence of a rash, especially in combination with other symptoms, requires immediate medical attention.
Sensitivity to Light: Photophobia, or sensitivity to light, is a common symptom of meningitis. Bright lights can cause discomfort and eye pain, leading individuals to avoid well-lit environments. If light sensitivity is experienced along with other warning signs, medical evaluation is essential.
Seizures: Seizures can occur in some cases of meningitis, particularly if the infection spreads to the brain. Seizures may manifest as convulsions, loss of consciousness, or uncontrolled movements. Any seizure activity warrants immediate medical attention.
Rapid Breathing and Difficulty Breathing: Meningitis can affect the respiratory system, leading to rapid breathing or difficulty breathing. This can be accompanied by chest pain, shortness of breath, or a sense of suffocation. If breathing difficulties are present, urgent medical care should be sought.
Irritability and Discomfort in Infants: In infants, the warning signs of meningitis may differ from those in adults. Infants may exhibit irritability, excessive crying, and general discomfort. They may refuse to eat, have a bulging fontanelle (soft spot on the top of the head), or have a stiff body. Any unusual behavior or discomfort in an infant should be evaluated by a healthcare professional.
Treatment options for Meningitis

Bacterial Meningitis Treatment
Bacterial meningitis is a medical emergency requiring immediate hospitalization and aggressive treatment. The mainstay of treatment involves:
a. Antibiotics: Intravenous (IV) antibiotics are administered as soon as possible to target the specific bacteria causing the infection. Broad-spectrum antibiotics are initially used until the causative organism is identified through laboratory tests. The choice of antibiotics is based on the local resistance patterns and the age of the patient.
b. Corticosteroids: In cases of bacterial meningitis caused by certain pathogens, such as Streptococcus pneumoniae, adjunctive corticosteroid therapy may be recommended. Corticosteroids help reduce inflammation and prevent complications, such as hearing loss and neurological damage.
c. Supportive Care: Alongside antibiotics, supportive care measures are implemented to manage symptoms and prevent complications. This includes intravenous fluids to maintain hydration, medications to control fever and pain, and close monitoring of vital signs and neurological status.
d. Isolation and Precautions: Patients with bacterial meningitis are placed in isolation to prevent the spread of infection. Healthcare professionals follow strict infection control measures, including wearing appropriate personal protective equipment (PPE) when caring for infected individuals.
Viral Meningitis Treatment
Viral meningitis is generally less severe than bacterial meningitis and often resolves on its own with supportive care. Treatment primarily focuses on:
a. Supportive Care: Rest, hydration, and over-the-counter pain relievers, such as acetaminophen or ibuprofen, are recommended to manage symptoms. Adequate rest and fluid intake help the body fight the viral infection and alleviate discomfort.
b. Antiviral Medications: In some cases, antiviral medications may be prescribed if the cause of viral meningitis is known and specific antiviral agents are available. However, most cases of viral meningitis do not require antiviral treatment.
c. Hospitalization: Depending on the severity of symptoms, viral meningitis may require hospitalization for close monitoring, especially in infants, young children, older adults, or individuals with weakened immune systems.
d. Isolation and Precautions: Similar to bacterial meningitis, individuals with viral meningitis may need to be isolated during the acute phase to prevent the spread of the virus. This is particularly important in healthcare settings where vulnerable populations may be at risk.
Additional Treatment Measures
In addition to specific treatments for bacterial or viral meningitis, there are additional measures employed to manage complications and support recovery:
a. Seizure Control: If seizures occur, anticonvulsant medications may be prescribed to control seizure activity and prevent further complications.
b. Ventilation Support: In severe cases of meningitis, respiratory support with mechanical ventilation may be necessary if breathing becomes compromised.
c. Monitoring and Neurological Assessment: Regular monitoring of vital signs, neurological status, and laboratory parameters helps evaluate the progress of treatment and identify any complications that may arise.
d. Follow-up Care: After the acute phase of meningitis, individuals may require follow-up care to assess their recovery, monitor for any long-term complications, and provide appropriate support and rehabilitation as needed.
Conclusion
In conclusion, meningitis is a potentially devastating condition that requires immediate attention and intervention. Timely diagnosis, prompt treatment, and preventive measures such as vaccination are crucial in combating this disease. Meningitis can cause severe complications, including neurological damage and even death, making awareness and education vital for early recognition and intervention. It is important for individuals to be familiar with the signs and symptoms of meningitis and seek medical attention promptly if they suspect an infection. By prioritizing prevention, early detection, and effective treatment, we can reduce the impact of meningitis and safeguard the health and well-being of individuals at risk.
Recent Articles

Find Top Ayurvedic Herbs for Memory and Cognitive Boost
In this day and age, where everything seems to go by fast, it is important to ensure that we maintain the sharpness of our minds. Due to the endless distractions and information overload, most individuals are facing problems with the inability to remember and concentrate, as well as brain fog. Ayurveda can be a fortunate way of treating memory and cognitive skills because they have original and time-proven natural enhancements. These primordial herbs are used in strengthening brain health, improving focus, and mental clarity, and have no side effects. This blog will discuss the best ayurvedic herbs that aid in learning, memory, and cognitive capabilities, to keep your mind alert and active at any age.Brahmi - The Brain Tonic of AyurvedaBrahmi (Bacopa monnieri) is a very famous Ayurvedic brain-healthy herb. This herb, which is often referred to as a herb of grace, has been used over the years to enhance memory and cognition naturally.How Brahmi Supports MemoryBrahmi improves brain action by promoting the synthesis of brain chemicals, which are associated with the learning and memory process. It is also helpful to students and other professionals who are required to remain on top and who are required to be focused. Brahmi causes a reduction in stress, which also contributes significantly towards the improvement of memory.Brahmi and Cognitive PsychologyCognitively, as a psychology of the mind, as well as memory, Brahmi aids in facilitating the quick or accelerated processing of information, as well as storing information for a longer period. It enhances the mind capacity, like keeping attention and problem-solving, which are important during learning.Usage of BrahmiBrahmi is available in powder, tablet, or syrup form. You can take it with warm milk or water in the morning. Some even prefer Brahmi oil massages to improve clarity and reduce anxiety.Shankhpushpi - For Mental Calmness and FocusShankhpushpi (Convolvulus pluricaulis) is another Ayurvedic herb praised for enhancing cognition and memory. It works by calming the mind and promoting peaceful sleep, which is vital for proper brain function.How Shankhpushpi Helps the BrainShankhpushpi improves memory by reducing mental fatigue, anxiety, and stress. It nourishes the nervous system and improves communication between brain cells, which aids learning, memory, and cognition.Shankhpushpi and Cognitive TherapyUsed as part of cognitive therapy for memory loss, Shankhpushpi is often prescribed by Ayurvedic practitioners to people suffering from memory issues caused by stress or aging. It enhances alertness while keeping the mind relaxed.How to Use ShankhpushpiIt is commonly taken as syrup or mixed with honey or milk. Regular intake shows noticeable improvement in memory and attention span.Ashwagandha - The Stress Buster for the BrainAshwagandha (Withania somnifera) is a powerful adaptogen that helps the body cope with physical and emotional stress. In Ayurveda, it is used to rejuvenate the body and boost brain power.How Ashwagandha Enhances MemoryAshwagandha helps improve memory and cognitive functions by reducing cortisol levels. Chronic stress is one of the main enemies of brain health. This herb helps protect brain cells from stress damage and improves mental performance.Ashwagandha in Cognition and Memory PsychologyIn cognition and memory psychology, Ashwagandha is known for improving attention, processing speed, and overall mental alertness. It's especially helpful for people facing burnout, fatigue, or age-related cognitive decline.Best Way to Take AshwagandhaAshwagandha is available in capsule, powder, or liquid extract form. Taking it with warm milk before bedtime helps in relaxing the mind and promoting sound sleep.Vacha - The Herb of Clarity and SpeechVacha (Acorus calamus) is a lesser-known but highly effective Ayurvedic herb for mental clarity and speech improvement. It stimulates the brain and improves communication skills, which are an important part of cognitive ability.Vacha's Role in Improving MemoryVacha improves cognition and memory by clearing mental fog and enhancing concentration. It is often used to support speech development in children and speech clarity in adults.Vacha and Learning Memory FunctionsIn the realm of learning, memory, and cognition, Vacha boosts the ability to absorb and retain new information. It's ideal for those who feel mentally sluggish or forgetful.How to Use VachaVacha powder can be taken with honey or ghee in small quantities. It should be used under guidance as it's quite potent and may not be suitable for everyone.Mandukaparni - The Natural Nerve TonicMandukaparni (Centella asiatica), also known as Gotu Kola, is another brain-friendly herb used in Ayurveda. Centella asiatica acts as a rejuvenator for the brain and nervous system.Mandukaparni's Effects on MemoryMandukaparni enhances memory and cognitive performance by promoting better circulation to the brain. It supports the growth of new brain cells, which is essential for long-term memory and learning.Mandukaparni and Cognitive DevelopmentIt supports cognition and memory psychology by helping in brain development and improving learning capacity. Children and students often benefit the most from this herb.Guduchi - The Detoxifier for Brain and BodyGuduchi (Tinospora cordifolia) is well-known for its immune-boosting and detoxifying effects, but it also has great benefits for brain health. Ayurveda regards it as a 'Medhya Rasayana'-a group of herbs that nourish the mind.How Guduchi Affects Brain FunctionGuduchi boosts memory and cognitive function by removing toxins from the nervous system. A cleaner system means better brain function, faster thinking, and more focus.Guduchi and Cognitive TherapyUsed as part of cognitive therapy for memory loss, Guduchi helps restore mental energy and improves the ability to handle emotional and physical stress.Jatamansi - The Memory RootJatamansi (Nardostachys jatamansi) is a calming herb with powerful effects on the brain. It works as a brain tonic and is often used in Ayurveda to support emotional balance.Jatamansi for Cognition and MemoryThis herb improves cognition and memory psychology by calming the nervous system and promoting emotional well-being. It is particularly helpful for people with insomnia, anxiety, or depression affecting their memory.Jatamansi's Role in LearningJatamansi supports learning, memory, and cognition by promoting healthy sleep and reducing brain fatigue. A well-rested brain is better at retaining and recalling information.Ayurvedic Practices to Support Brain HealthIn addition to herbs, Ayurveda recommends some daily habits and therapies to support memory and cognitive function.Abhyanga (Head Massage)Massaging the scalp with herbal oils like Brahmi or Jatamansi oil improves blood circulation to the brain and helps in better memory retention.Meditation and PranayamaBreathing techniques and meditation calm the mind, reduce stress, and increase focus. These are often part of cognitive therapy for memory loss in holistic healing systems.Final ThoughtsAyurveda has a healthy and natural method of enhancing memory and mental health. Brahmi, Shankhpushpi, Ashwagandha, Vacha, Mandukaparni, Guduchi, and Jatamansi are some of these ancient herbs, which are not only centuries old but are even supported further by modern science as described to help the brain. As a student, working professional, or an elderly individual who feels like keeping things on his or her toes, these are Ayurvedic herbs and practices that you can adopt to help you in your process of learning, remembering, and thinking. Good to remember to always take with instructions and correct dosages of an Ayurvedic practitioner, as to go along with, especially when mixed with medications that you are already on.

Discover Holy Basil Benefits for Immunity and Natural Calm
Tulsi or Holy Basil is considered one of the most precious herbs in traditional Indian medicine. The aromatic plant is also known as the Queen of Herbs, and it is popular due to its healing powers. Ayurvedic use Ayurvedic practices have been practiced over the centuries to treat stress, infections, and strengthen immunity. With the current busy lifestyle, the importance of the holy basil is increasing since people are trying to find natural products to help them live healthy and tranquil lives. Now, let us understand why holy basil is regarded as one of the best immune-boosting herbs and how you can consume holy basil in your daily life to enjoy better health and peace of mind.What Makes Holy Basil So Special?What is so special about Holy basil is that it is not an ordinary herb, and Holy basil is a super herbal adaptogen. Adaptogens are useful in adjusting your body to stress, anxiety, and fatigue. This is a plant rich in vitamins, antioxidants, and essential oils, which serve general well-being.Holy Basil and AyurvedaHoly basil is a sacred and curative plant as mentioned in the Ayurveda text. Now, Indian people often cultivate they also grow near their dwellings and temples, not only because of their therapeutic properties but also to protect their spiritual entities.Scientific Backing for Holy Basil BenefitsWhat the traditional medicine has always assumed is supported by modern research. Holy basil has antiviral, antibacterial, and anti-inflammatory compounds, namely, eugenol, ursolic acid, rosmarinic acid, and linalool.Top Holy Basil Benefits for the Immune System and Mental CalmHoly basil is not only good for your body but also for your mind. Here's how it helps you feel strong and relaxed.1. Boosts Immunity NaturallyOne of the major holy basil benefits is its immune-boosting ability. It helps the body produce more immune cells and fight infections.Rich in antioxidants: These help remove toxins and support cell repair.Fights bacteria and viruses: Holy basil can help reduce the severity and frequency of colds, flu, and other infections.Supports respiratory health: It is often used in herbal teas to ease coughs, bronchitis, and sore throats.2. Reduces Stress and AnxietyAs a holy basil herbal adaptogen, it reduces the levels of cortisol, the stress hormone.Helps you feel calmer and more centered.Improves sleep quality and reduces restlessness.Supports balanced moods during stressful situations.3. Supports Digestive HealthHoly basil promotes healthy digestion, making it useful for anyone dealing with indigestion, bloating, or constipation.Stimulates natural digestive enzymes.Reduces inflammation in the stomach lining.Acts as a mild laxative when needed.4. Enhances Brain FunctionTulsi may help improve memory and mental clarity. Its adaptogenic effects reduce brain fog and mental fatigue.Supports better focus and attention.May reduce symptoms of depression and anxiety.Protects brain cells from oxidative stress.5. Keeps Blood Sugar and Cholesterol in CheckRegular use of holy basil can help regulate blood sugar levels and improve heart health.Lowers bad cholesterol (LDL).Reduces blood pressure naturally.Enhances insulin function and blood sugar balance.Common Holy Basil Uses in Daily LifeYou don't have to be an herbalist to benefit from holy basil. It's available in many forms and can be easily added to your daily routine.1. Holy Basil TeaOne of the most popular holy basil uses is drinking it as a tea.Boil 5-10 fresh or dried leaves in water.Let it simmer for 5-10 minutes.Add honey or lemon for flavor.This tea is excellent for calming your nerves and boosting your immunity.2. Holy Basil SupplementsTulsi is available as capsules, tablets, or powders in health stores. These are great if you don't have access to fresh leaves.Always check the dosage instructions.Look for organic, high-quality sources.Consult your doctor if you're on medication.3. Cooking with Holy BasilAlthough not as common as sweet basil in Western cuisine, holy basil can be used in certain dishes, especially herbal soups and broths.Add to soups or stews for a healing boost.Use in herbal chutneys or sauces.4. Tulsi Essential OilThis oil can be used for aromatherapy or added to carrier oils for massage.Helps reduce stress when diffused.Can be added to bath water for relaxation.Holy Basil as One of the Best Immune-Boosting HerbsAmong all the immune-boosting herbs, holy basil stands out for its wide range of benefits. It not only strengthens your immune system but also helps your body recover faster from illnesses.1. Strengthens the Body's Defense SystemHoly basil supports the immune system by increasing the activity of helper cells and killer cells that destroy harmful pathogens.2. Fights Oxidative StressEnvironmental toxins, unhealthy diets, and stress lead to oxidative damage. Holy basil's antioxidants help protect the body from this damage.3. Anti-Inflammatory PowerChronic inflammation can weaken the immune system. Holy basil's natural anti-inflammatory compounds help reduce this risk.Why Holy Basil Herbal Adaptogens Are Gaining PopularityPeople today are turning toward natural remedies to cope with stress and maintain health. Holy basil herbal adaptogens are a key part of this movement.1. Adaptogens ExplainedAdaptogens help the body "adapt" to both physical and emotional stress. They balance hormones, regulate stress response, and restore energy.2. Holy Basil's Unique Adaptogenic RoleUnlike some other adaptogens that only work on stress, tulsi has a wide spectrum of healing.Balances cortisol.Calms the nervous system.Enhances focus and motivation.Long-term energy levels.3. Better than Synthetic AlternativesHoly basil works gently with your body and has little to no side effects. It's a natural option compared to synthetic stress-relief or immunity-boosting pills.Side Effects and PrecautionsHoly basil is generally safe, but here are a few things to keep in mind:1. Avoid in PregnancyPregnant women should avoid large doses of holy basil due to its possible effects on hormones.2. Medication InteractionsIf you are taking blood thinners, diabetes medication, or thyroid drugs, consult your doctor first.3. Allergic ReactionsAlthough rare, some people may be allergic to basil. Start with small amounts and watch for signs of irritation or discomfort.How to Grow Holy Basil at HomeWant fresh tulsi every day? It's easy to grow holy basil in a pot or garden.1. Choose a Sunny SpotHoly basil loves sunlight. Place the plant where it gets at least 4-6 hours of sunlight daily.2. Water ModeratelyWater when the topsoil feels dry. Do not overwater, as it can rot the roots.3. Harvest RegularlyPluck the leaves often to encourage new growth and to use them in teas or remedies.Final ThoughtsHoly basil is not only a conventional herb. It is a strong natural product that has the following positive effects of supporting your immune system, reducing stress, and supporting emotional balance. The holy basil benefits can be enjoyed in all kinds of forms, from drinking tulsi tea to consuming supplements. Whether it is to enhance the immune system of your body, or you simply need to relax and take a moment of peace in the hustle and bustle of your life, this queen of immune-enhancing herbs will find a place in your life.

Tai Chi Stretching Exercises for Stress and Stiffness
Stiff, tense, or having a thought overload? Tai Chi stretching will help restore balance between your body and mind. These slow movements are good to increase flexibility and relieve stress, and maintain well-being in general. Regardless of whether you are new to Tai Chi or seek minimalistic routines, this guide will take you through simple, easy-to-learn stretches that are based on the conventions of traditional Tai Chi. Why Choose Tai Chi for Stretching and Stress ReliefTai Chi is an ancient Chinese exercise that comprises deep breathing, slow movements, and meditation. Tai chi stretching exercises are performed at low intensities, unlike the high-impact exercises that are intensive and rough on the joints. This renders them ideal for individuals of all ages/fitness categories.Improves Flexibility and BalanceTai Chi stretches methods are slow and smooth, aiding in joint flexibility, building strength, and enhancing posture. With time, you will find there is improved balance and the body is less stiff.Reduces Mental and Physical StressTai Chi is also referred to as relaxation. Slow, deep rhythmic breathing combines with fluid movements that induce a meditative state, which drops levels of stress hormones as well as relaxes the entire nervous system.Safe for All AgesDue to the slow nature and low risk of injury, Tai Chi is an appropriate form of activity for seniors, newcomers, or individuals with injuries or persistent pain. It enables people to progress at their chosen speed and supports their strength, flexibility, and balance.Getting Started with Tai Chi Stretching ExercisesBefore diving into specific moves, it's important to warm up your body and understand the basic Tai Chi principles. These foundational tips will help you practice more effectively and safely.Start with Deep BreathingStand in a relaxed position. Breathe in slowly through your nose, letting your abdomen expand. Breathe out through your mouth. Repeat this for one to two minutes. This breathing style calms your mind and prepares your body for movement.Maintain Good PostureKeep your spine straight, shoulders relaxed, and knees slightly bent. Imagine a string pulling your head upward-this will help align your posture.Stay Grounded with Gentle MovementsTai Chi encourages smooth and flowing motion. Avoid jerky or quick actions.Simple Tai Chi Exercises for Stress ReliefThese simple tai chi exercises are easy enough for beginners but powerful enough to help release mental tension and bring clarity to your day.Cloud Hands (Yun Shou)Calms the mind, improves arm flexibility, and builds coordination.Stand with feet shoulder-width apart.Raise both arms to chest height, palms facing down.Slowly move both hands to the left while shifting your weight to the left leg.Reverse and move hands to the right while shifting weight.Repeat slowly for 10-15 rounds.Embrace the TreeEncourages deep breathing, mental health, and upper body relaxation.Stand tall with feet shoulder-width apart.Raise your arms in a rounded shape in front of your chest, like hugging a tree.Keep your elbows relaxed and palms facing you.Breathe deeply, hold the position for 2-3 minutes.Opening and Closing the ChestReleases tension in the shoulders and opens the heart area.Start with your arms by your sides.Inhale and raise arms sideways to shoulder level.Exhale and bring your hands in front of your chest as if pressing a ball.Repeat slowly for 10-12 repetitions.Basic Tai Chi Exercises for Body StiffnessWhen stiffness hits your neck, back, or legs, these basic tai chi exercises can help loosen tight muscles and restore body flow.Waist TurningLoosens the spine and reduces back tightness.Stand with feet shoulder-width apart, arms relaxed at sides.Slowly rotate your waist left and right, allowing your arms to swing naturally.Keep your knees soft and head facing forward.Do this for 1-2 minutes gently.Tai Chi Neck StretchRelieves neck stiffness and improves head mobility.Sit or stand comfortably.Slowly tilt your head to the right, feeling the stretch on the left side.Hold for 10 seconds, then switch sides.Repeat 3-4 times on each side.Knee CirclesIncreases flexibility in the knees and legs.Place your feet together, and bend your knees slightly.Put your hands on your knees and rotate them in circles.Do 10 circles clockwise, then 10 counterclockwise.Tai Chi Simple Exercises for Daily UseYou don't need a big space or a full routine to feel the benefits of Tai Chi. These simple tai chi exercises can be practiced at home, at work, or even during short breaks.Standing Meditation (Zhan Zhuang)Builds inner strength and calmness.Stand upright with knees slightly bent.Let your arms hang naturally or rest in front like holding a ball.Close your eyes, breathe slowly, and feel your body's natural energy.Stay in this position for 2-5 minutes.Shoulder RollsEases shoulder tension, especially for people who sit for long hours.Inhale as you lift your shoulders toward your ears.Exhale as you roll them back and down.Repeat 10 times, then reverse the direction.Energy Ball RotationImproves focus and arm flexibility.Hold your hands in front of your body like you're holding a ball.Slowly rotate the imaginary ball in small circles using both hands.Keep your movements soft and steady for 1-2 minutes.Building Your Tai Chi RoutineConsistency is key. You don't need to master all forms-just pick a few stretches and practice daily. With regular use, tai chi stretching exercises can become a healing part of your lifestyle.Morning RoutineStart your day with deep breathing, "Cloud Hands," and waist turning to wake up your body gently and boost circulation.Midday StretchAfter long hours at work or screen time, try shoulder rolls and neck stretches to refresh your energy and prevent stiffness.Evening Wind-DownUse "Embrace the Tree" or "Standing Meditation" to relax before bed. This helps quiet the mind and improve sleep quality.Helpful Tips for Practicing Tai Chi EffectivelyThe best way to benefit from Tai Chi is to stay mindful and relaxed during your practice. Here are a few practical tips to enhance your experience.Wear Comfortable Clothing: Loose, breathable clothes allow free movement and help you stay comfortable throughout the session.Choose a Quiet Space: A calm, peaceful setting-indoors or outdoors-can increase focus and relaxation.Listen to Your Body: If a stretch feels uncomfortable or causes pain, stop and adjust. Tai Chi is about harmony, not force.Final ThoughtsIn the modern competitive world, it is important to look at natural means to deal with stress and body aches. The stretching exercises in tai chi have a holistic approach. Simple to understand, greatly effective, and without any risk of age factor, they calm the mind and stretch the body simultaneously in a soothing way. The beauty of tai chi is that whether you are practicing some simple tai chi movements in your living room or establishing a complete program of simple tai chi movements, the results are actual and permanent. You will see a reduction in tensions, an increase in flexibility, and a calmer mental state in the course of time. Therefore, take it easy and relax, breathe in, breathe out, and make your everyday life turn into more and more Tai Chi.

How Bikram Yoga Can Transform Your Fitness Routine
When it comes to elevating your physical and mental health, few practices can rival the discipline and benefits of Bikram Yoga. Whether you're looking to increase flexibility, build endurance, detox your body, or simply improve your overall well-being, incorporating Bikram Yoga into your fitness routine could be a game changer.In this comprehensive guide, we'll dive into what is Bikram Yoga, explore essential Bikram Yoga poses, discuss its many advantages, and understand why so many fitness enthusiasts are embracing this powerful practice.What Is Bikram Yoga?Bikram Yoga is a specific type of hot yoga founded by Bikram Choudhury in the 1970s. The practice consists of a fixed sequence of 26 postures (asanas) and two breathing exercises, performed in a room heated to around 105°F (40°C) with 40% humidity. Each class lasts 90 minutes and follows the same sequence regardless of where you practice.The high temperature aims to mimic the climate of India, where yoga originated. It also helps in increasing flexibility, reducing the risk of injury, and promoting intense sweating for detoxification.Bikram Yoga BenefitsOne of the beautiful things about Bikram Yoga lies in the infinite range of health benefits it offers. Physical transformation, mental clarity, and emotional balance are just a few things it provides. Here is a detailed explanation of some of the Bikram Yoga benefits are: 1. FlexibilitySince the heat energizes the muscles, it allows possible deeper stretching and greater flexibility. With consistent practice, people begin to notice improvement in their range of motion around joints and muscles.2. DetoxificationHeavy sweating during every class flushes toxins out of your system. This detoxification supports the health of your skin and internal organs.3. Strength and ToningWith the absence of weights or fast movements, Bikram Yoga develops great strength galvanizing muscles throughout the body as they maintain Bikram yoga positions for extended durations.4. Posture and AlignmentAn important function of the Bikram series is to correct imbalances and improve posture by strengthening core, spine, and stabilizing muscles.5. Increased Focus on the MindWithstanding the heat and ensuring concentration on breath and movement, train the brain to focus and maintain composure under pressure.6. Stress Release and Emotional BalanceSimilar to any other yoga practice, it helps to foster the mind-body connection instrumental in stress relief, anxiety, and mood swings.7. Cardiovascular BenefitsWhile being a low-impact exercise, Bikram shares cardiovascular conditioning features with moderate aerobic exercise due to its production of intense environments.8. Weight LossRegular sessions can help burn calories and boost metabolism, making it easier to manage or reduce weight over time.Discover more: How Yoga Supports Mental Health and Reduces AnxietyBikram Yoga Poses: The 26 Asanas Bikram Yoga has a structured format of 26 poses each designed to develop certain muscle groups and organs. Together these poses provide an entire workout. Here is an overview of some of Bikram Yoga asanas and their associated benefits:1. Standing Deep Breathing (Pranayama)To oxygenate the body and prepare it for the workout.2. Half Moon Pose with Hands to Feet PosePromotes spine flexibility and strengthens the core, arms, and shoulders.3. Awkward PoseFocuses on the thighs, calves, and spine while developing balance and coordination.4. Eagle PoseIncreases flexibility in the hips, shoulders, knees, and ankles, and helps with circulation.5. Standing Head to Knee PoseExercises concentration, balance, leg-building, and abdominal muscles.6. Standing Bow Pulling PoseBuilds circulation, leg strength, and improves spine elasticity.7. Balancing Stick PoseBuilds cardiovascular strength and full-body alignment.8. Standing Separate Leg Stretching PoseStretches the spine and hamstrings and aids in digestion.9. Triangle PosePerhaps the one of the best for Bikram Yoga positions for flexibility, strength, and detoxification.10. Tree Pose and Toe StandBuild ankle strength and posture, and balance.11. Dead Body Pose (Savasana)Allows absorption of benefits by the body and resting in between the sequences.12. Wind-Removing PoseAssists digestion and massages the colon.13. Cobra PoseStrengthens the lower back and tones the buttocks.14. Bow and Locust PosesOpen chest and shoulders; strengthen the spine and legs.15. Fixed Firm PoseImproves flexibility of the knee and ankle; strengthens lower limbs. 16. Half Tortoise PoseEnhances mental clarity and balances blood pressure.17. Camel PoseOpens the chest, improving spine flexibility and relieving emotional tension.18. Rabbit PoseStretches the spine and calms the nervous system.19. Head To Knee Pose With Stretching PoseStimulates internal organs and helps with digestion.20. Spine Twisting PoseImproves spinal mobility and blood circulation.21. Blowing in Firm Pose (Kapalabhati)Lung cleansing and invigorating the body to close the session.Bikram Yoga Advantages Over Traditional YogaIf you are considering whether Bikram Yoga could be your path, consider its advantages over any other style of yoga or fitness regime:1. Consistency of StructureUnlike vinyasa and hatha where routines may vary, in Bikram you can expect the structure to remain predictable. This allows you to keep track of your own progress over time.2. Fully Integrated Body WorkoutThis class moves through all systems and parts of the body-from muscles to joints and from organic systems to glands-Hence the class gives a truly holistic workout.3. Detox and RecoveryThe heat of the room induces a profuse sweat, promoting toxin elimination and muscle repair. Bikram Yoga is the choice of many athletes for post-workout recovery.4. Mental and Physical ToughnessThe atmosphere is deliberately taxing. Getting through the heat builds up mental strength and grit that are essential to both fitness and life.Who Can Practice Bikram Yoga?Bikram Yoga is appropriate for every fitness level, keeping scope from beginner to the advanced practitioners. But, it does require being in a small mental sphere of mind-especially for the first few sessions. You must consult your doctor if pregnant, have cardiovascular problems, or are sensitive to extreme heat.Don't Miss: 5 things to Remember to Practice Safe Yoga and Avoid InjuriesTips for First-TimersIf you're planning for your first session, here are some tips to prepare you:Have plenty of water before and after class to replace the fluids lost through sweating.Show up earlier to get acclimatized to the heated atmosphere.Take comfortable clothing, which is light and breathable.Bring along your yoga mat, towel, and water bottle.How to Add Bikram Yoga to Your Fitness RoutineYou don't need to replace your entire workout plan. Bikram Yoga can complement other forms of fitness like weight training, cardio, or running. Aim for 2-3 sessions per week to start, and increase frequency as your stamina improves.Pair it with strength training to enhance flexibility and mobility.Use it on rest days as active recovery.Add it as your main workout if you're looking for a low-impact but high-benefit alternative.Explore more: Unlocking The Miraculous Benefits of Ashtanga Vinyasa YogaConclusionBikram Yoga is more than just a series of asanas-it's a transformative journey for the body and mind. From increased flexibility and detoxification to improved mental focus and cardiovascular health, the benefits of Bikram Yoga are numerous and well-documented.By committing to the practice, you'll not only notice physical improvements but also gain a deeper sense of discipline, self-awareness, and inner peace. Whether you're a seasoned athlete or someone starting fresh on your wellness journey, Bikram Yoga can completely reshape your fitness routine-one sweaty, focused session at a time.

Ashwagandha Benefits and How to Use It in Your Daily Routine
In a time of unending high productivity and digital overstimulation, many seek balance, clarity, and restoration from ancient natural remedies. Ashwagandha is one of the most researched and respected of these remedies and an adaptogenic herb that has been utilized in Ayurveda medicine for thousands of years. Ashwagandha is celebrated for its usefulness and medicinal efficacy, offering a holistic remedy for modern stress, fatigue and hormonal imbalance, and other ailments.What is Ashwagandha?Sapitionally, ashwagandha or Withania somnifera is a small evergreen shrub that is native to India, the Middle East, and parts of Africa. Its roots and berries are the source of medicinal tonics, powders, and extracts found in Ayurvedic medicine that have been reported to rewrite the energy in the mind and body. The word "ashwagandha" translates to "smell of a horse," in Sanskrit; this is probably a reference to its distinctive aroma as well as for the strength it is believed to bestow.This herb has been used for over 3,000 years to relieve stress, increase energy levels, and enhance concentration. Its adaptogenic qualities make it especially effective in helping the body manage stress responses by supporting adrenal function and promoting hormonal equilibrium. Rather than forcefully altering a biological system, Ashwagandha works to restore natural balance, which is why it remains such a trusted component in holistic health practices today.Learn More: Top 10 Herbs & Supplements: Depression Relief & StabilizersUnderstanding Adaptogenic HerbsThe idea of adaptogens is essential to understand the effects of Ashwagandha. Adaptogenic herbs are a class of restorative plants that help the body counteract the harmful effects of various physical, chemical, and biological stressors. These plants adapt their functionality based on your body's needs, whether this is tapping into the stimulatory effects to promote energy when fatigued or using the calming effects when unhinged.Adaptogens are different from pharmaceutical drugs, which target specific symptoms. Adaptogens can help address the fundamental problem of your body's stress system being out of balance because they support the body's hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis plays a systemic role in our body's response to stress. Ashwagandha has undergone more research than most adaptogens and is considered to be one of the most potent adaptogens. It acts as a natural modulator of cortisol (the primary stress hormone) in that it will support the uptake of challenges we face in a healthy manner while minimizing the ultimate wear and tear that chronic stress causes our body.One thing that makes adaptogens such as Ashwagandha so unique is their bidirectional activity. This means that they aren't just stimulatory or sedating but instead working with the body to adapt, normalize or more properly use their functions. Because of this, Ashwagandha may be the perfect herb for those who are dealing with anxiety, burnout, hormonal imbalances, sleep disturbances, and mental fog.Ashwagandha for Stress ReliefStress mitigation is nearly always the best-known, and most universally appreciated, of all the benefits of Ashwagandha. Chronic stress is not just a mind issue-it's a body issue that can impact digestion, the immune system, sleep quality, and cardiovascular health. When the stress hormone cortisol is chronically elevated, the effects can lead to mood destabilization, poor concentration, high blood pressure, and the potential for weight gain.Ashwagandha works to mitigate stress at both the physiological and psychological levels. Clinical trials consistently show that long-term use of ashwagandha extract reduces cortisol levels, especially in patients experiencing chronic anxiety or burnout. One study published in "Indian Journal of Psychological Medicine" found that participants who consumed high-concentration ashwagandha extract experienced a 44% reduction in stress and anxiety scores, compared with placebo subjects. Participants experienced an accompanying increase in sleep quality, levels of energy and improvement in their emotional wellbeing.This makes Ashwagandha an effective herbal alternative to pharmaceutical anti-anxiety medications, which often come with side effects or dependency risks. Daily supplementation of Ashwagandha may offer natural and sustainable relief for people dealing with long work hours, emotional upheaval, or frequent overwhelm.Exploring the 10 Benefits of Ashwagandha1. Natural Stress Reduction and Cortisol BalanceAs already mentioned, the ability of Ashwagandha to regulate cortisol levels is one of its signature qualities. Helping your body adapt to all kinds of stressors, whether acute or chronic, allows you to avoid descending into burnout, anxiety disorders, or immune suppression due to their potential prolonged presence. Following ingestion, many people find that their stress and anxiety responses are comparably calmer and more centered, often within a few days to weeks.2. Improved Sleep Quality and RelaxationIn this day and age of insomnia and restless sleep due to stressors, screen time, and disturbed circadian rhythms, we are all developing a better appreciation for sleep than ever. Ashwagandha contains some triethylene glycol (a natural compound that promotes sleep), that when consumed does not change sleep patterns like a sedative, instead it enhances your sleep quality by conserving your energy in addition to calming the nervous system and stabilizing nighttime cortisol spikes, making it easier to both fall asleep and stay asleep.Must Read: Adaptogens Ayurvedic Herbs for Weight Loss and Relaxation3. Enhanced Energy and VitalityIronically, while Ashwagandha helps promote better rest, it simultaneously improves energy levels and endurance in the daytime. Understanding that it positively affects mitochondrial function and adrenal control surrounding energy regulation. It emphasizes nourishing the body's vitality rather than overstimulating it, which is essential for those who suffer from general low energy, post-illness fatigue, and age-related physical decline.4. Improved Focus, Memory, and Cognitive FunctionAshwagandha also supports brain health. Research suggests it enhances memory, cognitive function, and information processing speed. This is due to its antioxidant effects in the brain and its role in regulating neurotransmitters such as serotonin and GABA. It may even protect against cognitive decline linked to aging or neurodegenerative disorders.5. Enhanced Immunity and ResilienceStress, poor diet, or long-term inflammation often undermines immune health. Ashwagandha increases natural killer cell activity, supports white blood cell production, and greatly reduces illness and improves infection recovery.6. Hormonal Balance for Men and WomenAshwagandha has been demonstrated to influence hormonal activity positively. In men, it increases testosterone, sperm count, and motility. In women, ashwagandha may offer relief from PMS symptoms, regulating the cycle, and fertility matters regarding stress or thyroid dysfunction. This ability to balance hormones is especially relevant during menopause or with adrenal exhaustion.7. Anti-Inflammatory and Antioxidant PropertiesChronic inflammation is at the root of so many of the chronic diseases we see today, such as, arthritis, diabetes, and heart disease. Ashwagandha decreases the levels of inflammatory markers, such as CRP (C-reactive protein), and it is rich in antioxidant properties to protect the stones in oxidative stress. For those seeking preventative health and longevity, ashwagandha is a great addition to long-term supplemental intake.8. Cardiovascular Benefits and Heart HealthAshwagandha can positively affect the health of the heart by lowering blood pressure, cholesterol values, and improving circulation. This is primarily from its anti-inflammatory and stress-relieving properties.Check This Out: Best Antiviral Herbs To Heal And Boost Your Immune System9. Muscle Growth and Physical PerformanceFitness enthusiasts increasingly turn to Ashwagandha to improve strength, stamina, and muscle recovery. Studies show it increases muscle mass and decreases body fat with resistance training. It also lowers exercise-induced muscle damage, helping with faster post-workout recovery.10. Enhanced Emotional Well-being and Mood StabilityLastly, Ashwagandha helps regulate mood and emotional resilience. Its impact on serotonin pathways and cortisol regulation makes it an effective herb for managing symptoms of depression, mood swings, and emotional fatigue. It creates a sense of balance and inner calm, supporting emotional stability in facing life's challenges.How to Use Ashwagandha in Your Daily RoutineThe great thing about Ashwagandha is how easily it can be taken as part of your day-to-day life. Whether you take them as capsules (my preference), drink it as tea, or blend it in smoothies, there are a variety of options to suit your lifestyle and schedule. Typically, the traditional form of Ashwagandha is powder. In Ayurveda, the powder is blended with warm milk, a pinch of turmeric and a spoon of honey into a soothing bedtime drink. Others blend the powder into smoothies or energy balls in the morning, especially if they are looking for some of Ashwagandha's invigorating benefits during the day. Capsules or tablets are the most convenient forms of Ashwagandha, as they are often standardized at specific doses for concentrations of withanolides. Because they are convenient, they are good for people who travel; or busy lifestyles. Generally, the best time to take, capsules or tablets is based on your unique needs - take in the morning for more energy and focus and at night if you are looking for calming effects to aid relaxation or sleep.While Ashwagandha tea can be enjoyed on its own, it can also be combined with other calming herbs such as chamomile, tulsi, or some licorice for a particularly soothing herbal tea. Drinking ashwagandha tea in the evening will help soothe the nervous system and prepare you for a restful night's sleep.Using tinctures or liquid extracts of ashwagandha is a quick and quickly absorbed option that can be mixed with water or juice. Tinctures and liquid extracts of ashwagandha are extremely potent and best used with the guidance of a health care professional if you need to take a higher therapeutic dose.Ayurvedic massage practice uses topical ashwagandha oil or ghee for the purpose of enhancing physical calmness while also balancing the nervous system. Given the high rates of body tension and anxiety experienced by so many people today, this may serve the purpose of balance and grounding to help alleviate a state of nervous exhaustion during or after a busy routine.Also Read: Ashwagandha: Learn Its Benefits, Side Effects And MoreConclusionAshwagandha is not a passing fad in health and well-being-it is a time-tested herbal ally that continues to show its value in today's wellness landscape. Whenever there is a notion of helping the body tolerate stress more efficiently, heightening energy levels, regulating hormone production and keeping the mind sharp will help people balance, feel resilient and live life differently. Given its versatility, I believe ashwagandha can offer gentle and enduring support when needed and bring profound support for emotional burnout, sleeping challenges, physical fatigue or days of busyness.

Add Your Comment Here